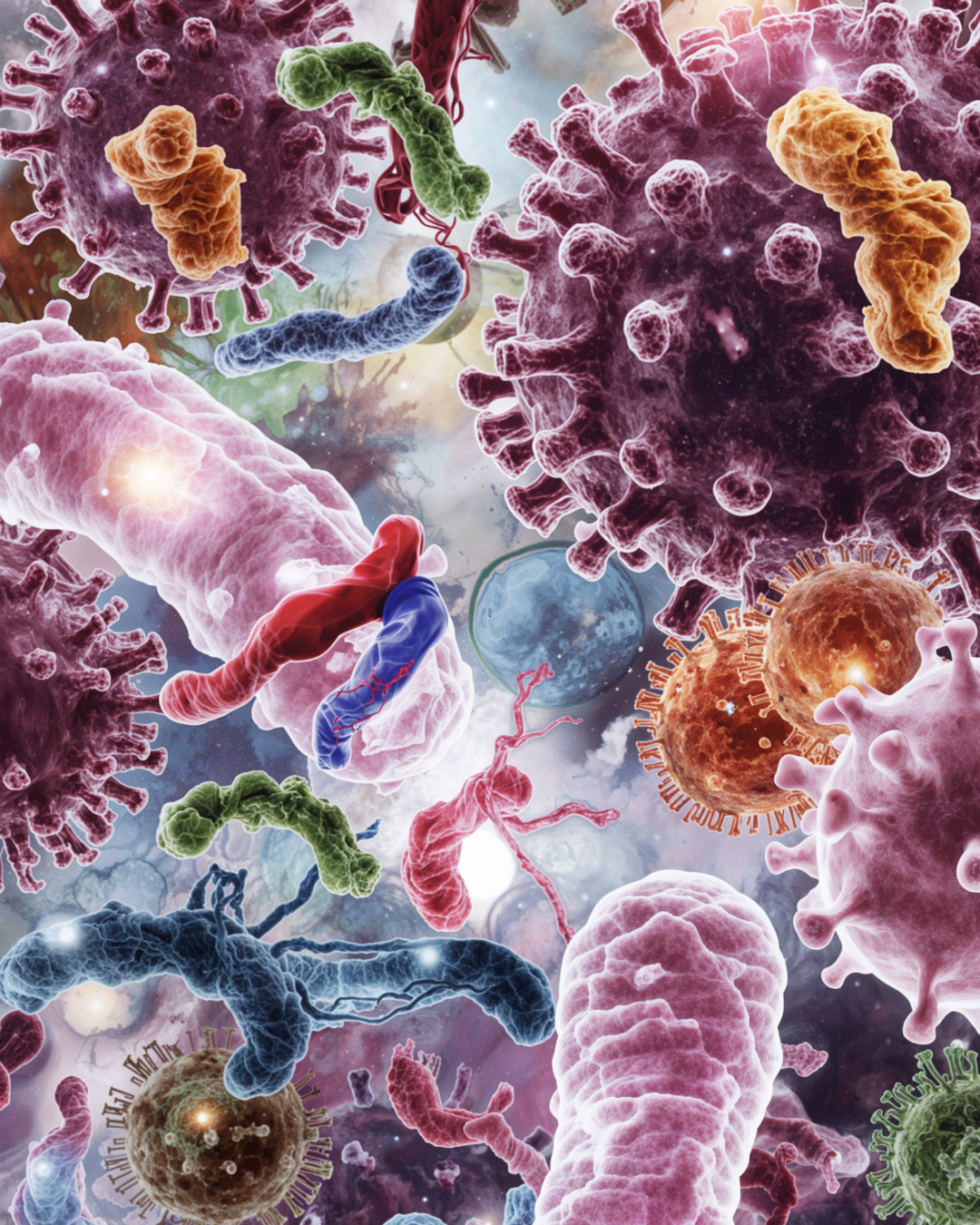
In recent years, science has uncovered an intricate connection between the gut and almost every system in the body — from the brain to the skin and now, even the lungs. This bi-directional communication, known as the gut-lung axis, offers fascinating insight into how digestive health profoundly influences respiratory wellbeing, immunity, and inflammation. Understanding this relationship opens new avenues for addressing conditions like asthma, chronic bronchitis, allergies, and even viral infections.
How the Gut and Lungs Communicate
The gut and lungs may seem like separate organs, but they’re connected through the mucosal immune system and the microbiota — the diverse community of bacteria, fungi, and other microorganisms that live in the gut and respiratory tract.
-
Immune Crosstalk: Immune cells activated in the gut can migrate through the bloodstream and influence the immune environment of the lungs.
-
Microbial Metabolites: Short-chain fatty acids (SCFAs) produced by gut bacteria — particularly butyrate, propionate, and acetate — have systemic anti-inflammatory effects that reach the lungs.
-
Inflammatory Mediators: Dysbiosis (an imbalance in gut bacteria) can increase systemic inflammation, contributing to respiratory disorders like asthma or COPD.
Essentially, what happens in the gut doesn’t stay in the gut — it echoes throughout the body, including the lungs.
How Gut Health Affects Lung Function
1. Immune Regulation
A balanced gut microbiome helps train the immune system to respond appropriately to pathogens without overreacting. When gut dysbiosis occurs, this balance is disrupted, often resulting in excessive inflammation in the lungs or heightened allergic responses.
2. Protection Against Respiratory Infections
Healthy gut bacteria enhance mucosal immunity, supporting the production of IgA antibodies and other immune defences that protect both the digestive and respiratory tracts. Studies have shown that individuals with diverse gut microbiota tend to experience fewer and milder respiratory infections.
3. Inflammation and Chronic Lung Conditions
Conditions like asthma, COPD, and chronic bronchitis are associated with systemic inflammation. A leaky gut or dysbiotic microbiome can perpetuate this inflammation, worsening respiratory symptoms and reducing tissue healing capacity.
How Lung Health Influences the Gut
The gut-lung axis works in both directions. Chronic respiratory inflammation, infections, or even the use of inhaled corticosteroids can alter the gut microbiome. For instance, individuals with long-term asthma or frequent antibiotic use often display reduced gut microbial diversity, which in turn can weaken gut barrier integrity and immune regulation.
Additionally, respiratory infections can change intestinal permeability and microbial composition — meaning that every cold or flu can have downstream effects on gut health.
The Role of the Microbiome in the Gut-Lung Axis
A thriving microbiome supports the gut-lung axis by:
-
Producing SCFAs that reduce airway inflammation
-
Regulating T-regulatory cells (Tregs) for immune balance
-
Supporting mucosal barrier integrity in both gut and lung linings
-
Inhibiting the growth of pathogenic microbes
On the other hand, a microbiome depleted by poor diet, stress, antibiotics, or environmental toxins can send distress signals that drive inflammation and immune dysregulation.
Strategies to Support the Gut-Lung Axis
1. Nourish the Microbiome
-
Include a variety of plant fibres (legumes, whole grains, fruits, and vegetables) to feed beneficial bacteria.
-
Consume fermented foods such as sauerkraut, kimchi, kefir, and yoghurt.
-
Consider a broad-spectrum probiotic to restore microbial diversity.
2. Reduce Inflammation
-
Focus on omega-3 fatty acids (found in flaxseed, algae, hemp, chia, and oily fish) to balance immune responses.
-
Limit refined sugars and processed foods, which promote dysbiosis.
-
Support the gut barrier with glutamine, zinc, and collagen peptides.
3. Support Detoxification and Liver Function
The liver plays a key role in managing inflammation and detoxifying endotoxins produced by an imbalanced microbiome. Support this with cruciferous vegetables, turmeric, and adequate hydration.
4. Strengthen Mucosal Immunity
-
Vitamin A, D, and C, they both support epithelial health and immune resilience.
-
Functional mushrooms (like reishi, cordyceps, and shiitake) enhance microbiome activity in both gut and lungs.
5. Breathe Well and Move
Gentle movement and deep breathing exercises increase oxygen flow, lymphatic circulation, and microbiome diversity. Regular outdoor time in natural environments also exposes the body to beneficial microbes.





Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.